
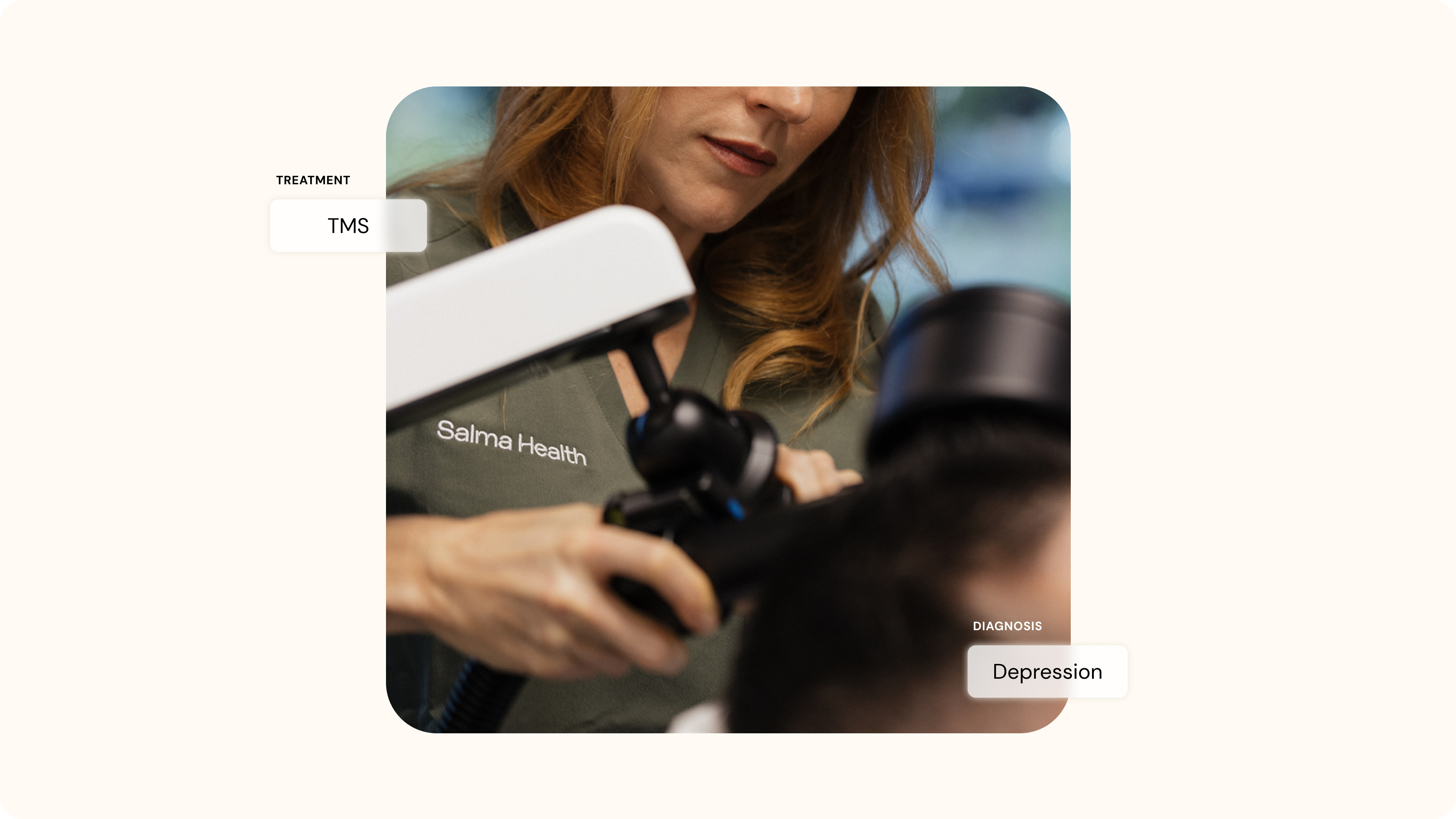
Can You Combine TMS with Antidepressants? Yes. TMS May be a Powerful Addition to Your Treatment Plan.
Many people experience only partial relief from antidepressants alone. TMS can be safely combined with medication to support brain circuits involved in mood regulation and may help people move closer to lasting remission.
.png)
If you’ve been taking antidepressants for some time but still feel weighed down by depression, you’re not alone. Many people living with major depressive disorder (MDD) reach a point where medication helps with some symptoms but never fully restores their sense of balance and well-being.
Antidepressants can steady the day, ease certain emotional burdens, and support sleep or appetite, yet for many people, the heaviness of depression still lingers. National outcomes data show that about one-third of people with MDD achieve relief from their depression after their first antidepressant trial, according to the National Institute of Mental Health. Research shows that each additional antidepressant trial is associated with diminishing chances of remission, which helps explain why many people continue to struggle even after multiple medication changes.
When Progress Stalls, Exploring Additional Options
When progress stalls, many people begin exploring additional treatment options. One of the most effective and well-studied options is Transcranial Magnetic Stimulation (TMS). Often, one of the first questions people ask is whether they need to stop their antidepressant before starting TMS therapy.
Clinically, the answer is almost always no. Research supports continuing antidepressants during TMS in most cases, as combination treatment is common and well tolerated.
Mohammed Ahmed, M.D., a neuropsychiatrist and clinical director at Salma Health, emphasizes that TMS is not designed to abruptly replace medication; rather, it is often used alongside medication, particularly in individuals who have experienced only partial benefit from pharmacologic treatment.
“TMS does not replace medication. But sometimes, it allows us to see what the medications have been trying to achieve,” says Dr. Ahmed.
Most individuals referred for TMS therapy have already tried two or more antidepressants at adequate doses and durations, which is a common definition of treatment-resistant depression. Continuing medication during TMS is not about promoting indefinite medication use, but about maintaining emotional stability while the brain undergoes neuromodulation, he explains.
How TMS and Antidepressants Work Together in the Brain
TMS uses magnetic pulses to stimulate networks in the brain responsible for mood regulation. Research has shown that these networks often function differently in people with depression.,
Common antidepressant medications target levels of certain neurotransmitters, such as serotonin or norepinephrine. TMS strengthens activity in mood-regulating circuits by supporting synaptic plasticity, which, in simple terms, is how the brain learns, adapts and recovers. When the two are combined, the brain receives support across chemical and circuit-based systems, which often leads to more meaningful improvement for people with treatment-resistant symptoms.
A common concern for people is whether continuing medication during TMS means they will need to remain on it indefinitely. Dr. Ahmed emphasizes that this is not necessarily the case.
“In my practice, we don’t change anything for about six months,” he says. “If someone achieves remission and maintains stability, then we may begin to carefully attempt to take them off medication.”
This approach aligns with established clinical guidelines, which emphasize sustained remission before medication tapering is considered. Many people have been on medication for years, and the brain adapts to those levels of neurotransmitter support. Stopping abruptly can trigger what is known as antidepressant discontinuation syndrome, which may involve dizziness, irritability or a sudden return of depressive symptoms.
“Tapering is always individualized,” he says. “It depends on the person’s history, coping skills and stability. We taper slowly because we want the brain to hold onto the gains.”
One of the most helpful concepts Dr. Ahmed shares is that TMS creates what he calls a therapeutic window. When symptoms begin to lift, people often notice that they can think more clearly, feel more energy, and re-engage with parts of daily life that had felt out of reach. He describes TMS as a beautiful tool that opens that window and gives people room to breathe again. The opportunity, he says, is what someone does with that opening. Turning that window into a door means using that period of clarity to build routines and supportive habits that help progress last.
The science supports this experience. When mood improves even slightly, the brain becomes more receptive to change. TMS research indicates that neuromodulation increases neuroplasticity, thereby making mood-regulating circuits more flexible and responsive.
.png)
Precision Neuromodulation and the SAINT® Approach
Researchers from the Stanford Brain Stimulation Lab (BSL) have demonstrated that depression can be more effectively treated by precisely targeting specific brain networks. In particular, their work focused on the circuit connecting the dorsolateral prefrontal cortex (DLPFC) and the subgenual cingulate (sgACC), a pathway associated with treatment-resistant depression. Building on this insight, researchers at the Stanford BSL developed SAINT® neuromodulation therapy (Stanford Accelerated Intelligent Neuromodulation Therapy), demonstrating that restoring functional activity within the DLPFC-sgACC circuit is associated with rapid symptom improvement in people with severe, treatment-resistant major depression.
For many people who have lived with depression for years, medication alone may bring partial relief but not full recovery. TMS offers a noninvasive, evidence-based option that directly targets mood circuits and increases the brain's receptivity to change.
For individuals who have struggled to progress beyond partial response, TMS can provide the momentum needed to achieve remission. If you are currently taking antidepressants and still searching for relief, TMS may be a powerful addition to your treatment plan.
1. https://www.nimh.nih.gov/funding/clinical-research/practical/stard/allmedicationlevels
2. https://pubmed.ncbi.nlm.nih.gov/33289425/
3. https://pubmed.ncbi.nlm.nih.gov/20439832/
4. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370%2824%2900339-0/fulltext
5. https://pubmed.ncbi.nlm.nih.gov/31638723/
6. https://www.health.harvard.edu/blog/transcranial-magnetic-stimulation-for-depression-2018022313335
7. https://pubmed.ncbi.nlm.nih.gov/34711062/
8. https://pmc.ncbi.nlm.nih.gov/articles/PMC5846193/
9. https://my.clevelandclinic.org/health/diseases/25218-antidepressant-discontinuation-syndrome
10. https://pubmed.ncbi.nlm.nih.gov/34711062/
Why Salma Health?
With locations in La Jolla, Laguna Hills, and the Bay Area, Salma Health offers advanced mental and behavioral health care in California, with both in-person and virtual options. We support individuals living with depression, anxiety, PTSD, OCD, brain injuries, and related conditions, using personalized, science-backed approaches.
Start Your Journey Today
Getting started doesn’t have to be overwhelming. You can begin with a 15-minute Care Options Call, connect with our care team, complete a comprehensive intake, or schedule online. We meet you where you are and build care around your needs. Schedule your first appointment today and experience a higher standard of brain care—grounded in science, clarity, and continuity.

.avif)
.avif)